First aid - Fainting:
Introduction:
Fainting is a brief episode of unconsciousness caused by a sudden drop in blood pressure. The most likely cause of this sudden drop will either be some change in the blood vessels or the heartbeat itself.
Blood vessels continually adjust their width to ensure a constant blood pressure. For instance, the vessels constrict (tighten) when we stand up to counteract the effects of gravity. Temporary low blood pressure can be caused by various events that prompt blood vessels to dilate (expand), including extreme heat, emotional distress or pain. The lack of blood to the brain causes loss of consciousness.
Most fainting will pass quickly and won’t be serious. Usually, a fainting episode will only last a few seconds, although it will make the person feel unwell and recovery may take several minutes. If a person doesn’t recover quickly, always seek urgent medical attention.
What is fainting?
Fainting is a sudden, brief loss of consciousness. When people faint, or pass out, they usually fall down. After they are lying down, most people will recover quickly.
The term doctors use for fainting is syncope (say "SING-kuh-pee").
Fainting one time is usually nothing to worry about. But it is a good idea to see your doctor, because fainting could have a serious cause.
What causes fainting:
Fainting is caused by a drop in blood flow to the brain. After you lose consciousness and fall or lie down, more blood can flow to your brain so you wake up again.
The most common causes of fainting are usually not signs of a more serious illness. In these cases, you faint because of:
- The vasovagal reflex, which causes the heart rate to slow and the blood vessels to widen, or dilate. As a result, blood pools in the lower body and less blood goes to the brain. This reflex can be triggered by many things, including stress, pain, fear, coughing, holding your breath, and urinating.
- Orthostatic hypotension, or a sudden drop in blood pressure when you change position. This can happen if you stand up too fast, get dehydrated, or take certain medicines, such as ones for high blood pressure.
Fainting caused by the vasovagal reflex is often easy to predict. It happens to some people every time they have to get a shot or they see blood. Some people know they are going to faint because they have symptoms beforehand, such as feeling weak, nauseated, hot, or dizzy. After they wake up, they may feel confused, dizzy, or ill for a while.
Some causes of fainting can be serious. These include:
- Heart or blood vessel problems such as a blood clot in the lungs, an abnormal heartbeat, a heart valve problem, or heart disease.
- Nervous system problems such as seizure, stroke, or TIA.
Sometimes the cause is unknown.
When is fainting the sign of a serious problem?
Fainting may be the sign of a serious problem if:
- It happens often in a short period of time.
- It happens during exercise or a vigorous activity.
- It happens without warning or if it happens when you are already lying down. (When fainting is not serious, a person often knows it is about to happen and may vomit or feel hot or queasy.)
- You are losing a lot of blood. This could include internal bleeding that you can't see.
- You feel short of breath.
- You have chest pain.
- You feel like your heart is racing or beating unevenly (palpitations).
- It happens along with numbness or tingling on one side of the face or body.
Reasons Why a Casualty Might Faint:
It can be triggered by any of the following:
• emotional shock
• pain
• over-exertion
• exhaustion
• lack of food
• dehydration
• sight of blood
• standing immobile in hot conditions
• standing up suddenly (particularly for the pregnant or elderly)
• heart rhythm changes or underlying heart conditions
Fainting Symptoms
Unconsciousness is an obvious sign of fainting.
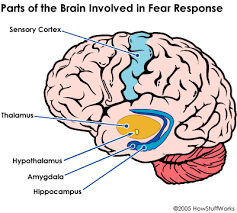
Vasovagal syncope:
- Before fainting, the person may feel light-headed and shaky and experience blurred vision.
- The person may "see spots in front of their eyes."
- During this time, observers note paleness, dilated pupils, and sweating.
- While unconscious, the person may have low pulse rate (less than 60 beats/minute).
- The person should quickly regain consciousness.
- Many people have no warning signs before a fainting (syncopal) episode.
Situational syncope:
- Consciousness returns when the situation is over, usually very quickly.
Postural syncope:
- Prior to the fainting episode, the person may have noted a blood loss (black stools, heavy menstrual periods) or fluid loss (vomiting, diarrhea, fever).
- The person may have experienced light-headedness when sitting or standing.
- Observers may note paleness, sweating, or signs of dehydration (dry lips and tongue).
Cardiac syncope: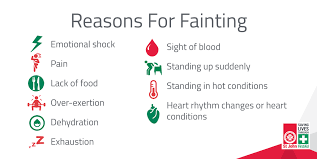
- The person may report palpitations (awareness of pounding, fast, or abnormal heartbeat), chest pain, or shortness of breath.
- Observers may note a weak, abnormal pulse, paleness, or sweating.
- Fainting often occurs without warning or following exertion.
Neurologic syncope:
- The person may have a headache, loss of balance, slurred speech, double vision, or vertigo (a feeling that the room is spinning).
- Observers note a strong pulse during the unconscious period and normal skin color.
Causes of a drop in blood pressure:
A temporary drop in blood pressure can be caused by different factors, including:
- Prolonged standing
- Extreme heat, which pushes blood away from the main circulatory system and into the vessels of the skin
- Emotional distress
- Severe pain
- The sight of blood
- The sight of a hypodermic needle
- Other events that a person may find distressing.
What exams and tests might you need?
To find the cause of fainting, a doctor will do a physical exam and ask questions about the fainting episode. You can help your doctor by being prepared to describe what happened before you fainted, how long you were "out," and how you felt when you woke up.
Depending on what the physical exam shows, the doctor may want to do tests. These tests may include:
- Blood tests.
- Heart tests such as ECG, ambulatory monitoring (with a Holter monitor or event monitor, for example), echocardiogram, or an exercise stress test.
- A tilt table test. This test checks how your body responds to changes in position.
- Tests for nervous system problems, such as CT scan of the head, MRI of the brain, or EEG.
How to Manage Faintness:
Usually people recover quickly, often within seconds, without lasting e¬ffects. However, if fainting is the result of an underlying medical condition or is recurrent, the casualty should see a doctor.
Here are the steps to follow for fainting:
1. Follow DRSABCD. If the casualty is not breathing it could be sudden cardiac arrest.
2. Loosen any tight clothing that could be restricting their breathing
3. Ensure there is plenty of fresh-air – open a window if possible
4. When the casualty becomes is conscious, lie them on their back and raise and support their legs. Kneel down next to them and raise their legs by placing a pillow under their calves. Watch their face for signs that they’re recovering. For a woman in advanced pregnancy, place padding under right buttock to tilt.
5. Treat any injury resulting from a fall.
What should you do about fainting:
If you know you tend to faint at certain times (such as when you get a shot or have blood drawn), it may help to:
- Sit with your head between your knees or lie down if you feel faint or have warning signs such as feeling dizzy, weak, warm, or sick to your stomach.
- Drink plenty of fluids so you don't get dehydrated.
- Stand up slowly.
If you feel faint:
- Lie down or sit down.
- If you sit down, place your head between your knees.
Discuss recurrent fainting spells with your doctor.
If someone else faints:
- Position the person on his or her back. Make sure the legs are elevated, if possible above the heart level.
- Check the person's airway to be sure it's clear. Watch for vomiting.
- Check for signs of circulation (breathing, coughing or movement). If absent, begin CPR. Call or your local emergency number. Continue CPR until help arrives or the person responds and begins to breathe.
- Help restore blood flow. If the person is breathing, restore blood flow to the brain by raising the person's legs above the level of the head. Loosen belts, collars or other constrictive clothing. The person should revive quickly. If the person doesn't regain consciousness within one minute, call for emergency medical assistance.
Fainting Self-Care at Home: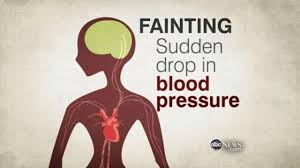
- If possible, help the person who has fainted to the ground to minimize injury.
- Stimulate the person vigorously (yelling, briskly tapping). Call emergency number immediately if the person does not respond.
- Check for a pulse and begin CPR, if needed.
- After the person recovers, encourage him or her to lie down until medical help arrives. Even if you believe the cause of the fainting is harmless, have the person lie down for 15-20 minutes before attempting to get up again.
- Ask about any persistent symptoms, such as headache, back pain, chest pain, shortness of breath, abdominal pain, weakness, or loss of function, because these may indicate a life-threatening cause of the fainting.
Fainting Follow-up
- If the cause of fainting or syncope is not determined, and the affected person is not hospitalised, he or she should see a health care practitioner within a few days. Learn to check your own pulse and teach your family members what to do in case you faint again.
- Many people never faint again after the first time.
- The affected individual may be referred to a heart specialist if cardiac syncope is suspected.
- If neurologic disease is suspected during the emergency department evaluation, the person should be referred to a neurologist.
Preventing Faintness:
If you feel yourself becoming faint, lie down on the ground until the feeling passes. This will stop you from hurting yourself. Other ways to help yourself if you feel faint are:
1. Keep hydrated with plenty of water
2. Don’t get up too quickly from lying or sitting down
3. Control your breathing
4. Controls triggers such as phobias (e.g. needles)
First aid- some one got faint
Fainting causes and treatment